The accreditors of this session require that you periodically check in to verify that you are still attentive. Please click the button below to indicate that you are.
624
<i>THE “PAN-UTILITY” OF ANORECTAL MANOMETRY IN PEDIATRIC AGE GROUP: RECOGNIZING CONSTIPATION VARIANTS, DECISION OF ESTABLISHING GUT CONTINUITY AND DISCRIMINATING ORGANIC FROM FUNCTIONAL CONSTIPATION </i>
Date
May 8, 2023
Explore related products in the following collection:
Society: AGA
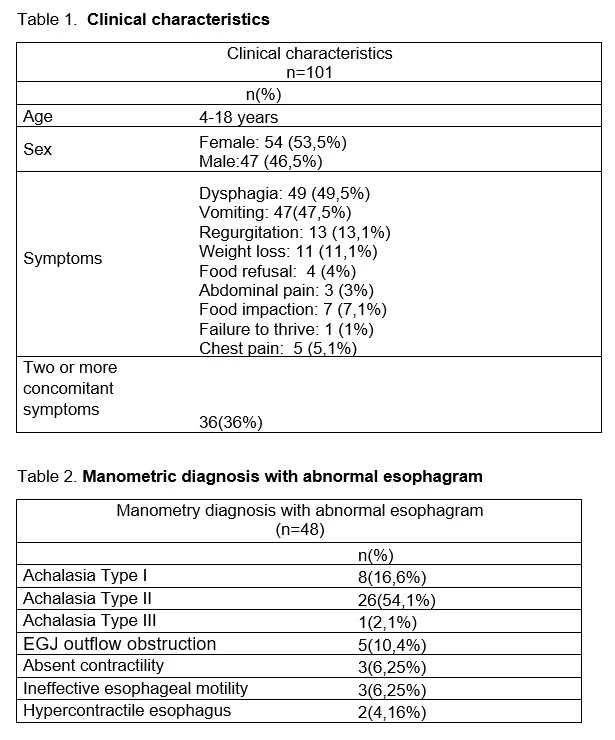
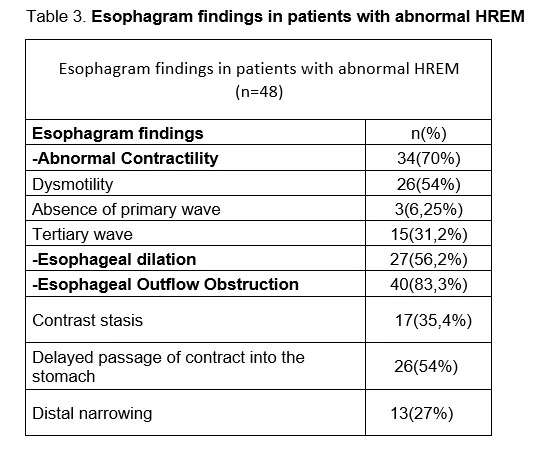
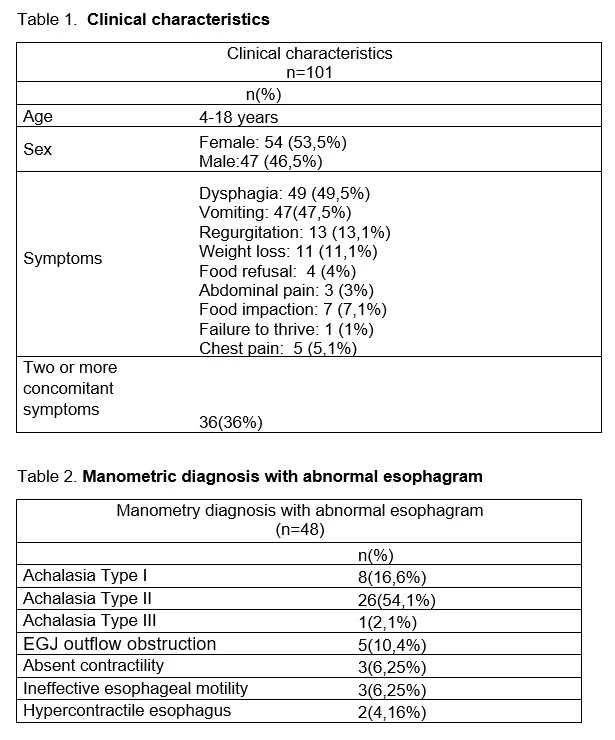
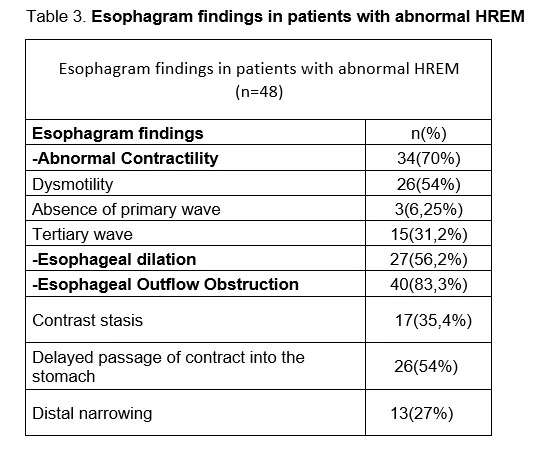
HREM is the gold standard for esophageal motility disorders with a PPV 96%, sensitivity 100% and specificity 98%. This study compares the barium esophagogram results with HREM in pediatric patients. Methods : Observational, retrospective, test-retest concordance study. Pediatric patients that had a barium esophagram performed within 90 days of the HREM were included. Results : A total of 101 patients with a median age of 13.6 years, (54 females) were analyzed. The most frequent symptoms were dysphagia, followed by vomiting, regurgitation and weight loss (Table 1). 60 patients had abnormal esophagram. (Abnormal contractility 66%, esophageal dilatation 50% and esophageal outflow obstruction 75%) 81.4% of abnormal esophagrams were consistent with an abnormal HREM, sensitivity of 92.3% and specificity of 90% (p<0.005). Ouflow obstruction on esophagogram is significantly associated with an abnormal IRP on HREM (p p<0.005) accuracy of 88%, sensitivity of 80.9% and specificity of 84.7%. Abnormal Distal Contractile Integral (DCI) on HREM is significantly associated with abnormal contractility on esophagram 72% accuracy, 63% sensitivity and 71.6% specificity (p=0.000) and with esophageal dilatation 57.8% sensitivity, 76.4% specificity and 74% accuracy (p<0.005) (Table 3). We found a good concordance between tests with a Kappa index of 0.69 (p<0.005) 11 patients had abnormal esophagram and a normal HREM and 6 had normal esophagram and abnormal HREM (including 2 type II achalasia) Discussion: Different tools allow evaluation of esophageal anatomy and motility; the barium esophagram is useful, minimally invasive and inexpensive. It is a valuable test for structural and functional evaluation of the esophagus, we found a sensitivity of 92% and specificity of 90% for the diagnosis of motor disorders, similar finding reported by Ott DJ et al. with a sensitivity of 89% and specificity of 91% in adult patients with dysphagia. All esophagrams with contrast stasis had abnormal HREM. Outflow obstruction in esophagram was associated with an abnormal IRP and dysmotility in esophagram with an abnormal DCI. Halland et al. found that isolated tertiary waves on esophagogram in patients without dysphagia is rarely associated with significant motor disturbances, we had only one patient with isolated tertiary waves and had a normal HREM. However, we found that out of 17 patients with non-isolated tertiary waves 2 had normal HREM, and 13 had achalasia. Conclusion: This study determined a good concordance between barium esophagram and HREM. Abnormal findings on esophagogram dysmotility, dilatation, and contrast stasis are significantly associated with abnormal HREM. A normal esophagram does not rule out a major motility disorder.
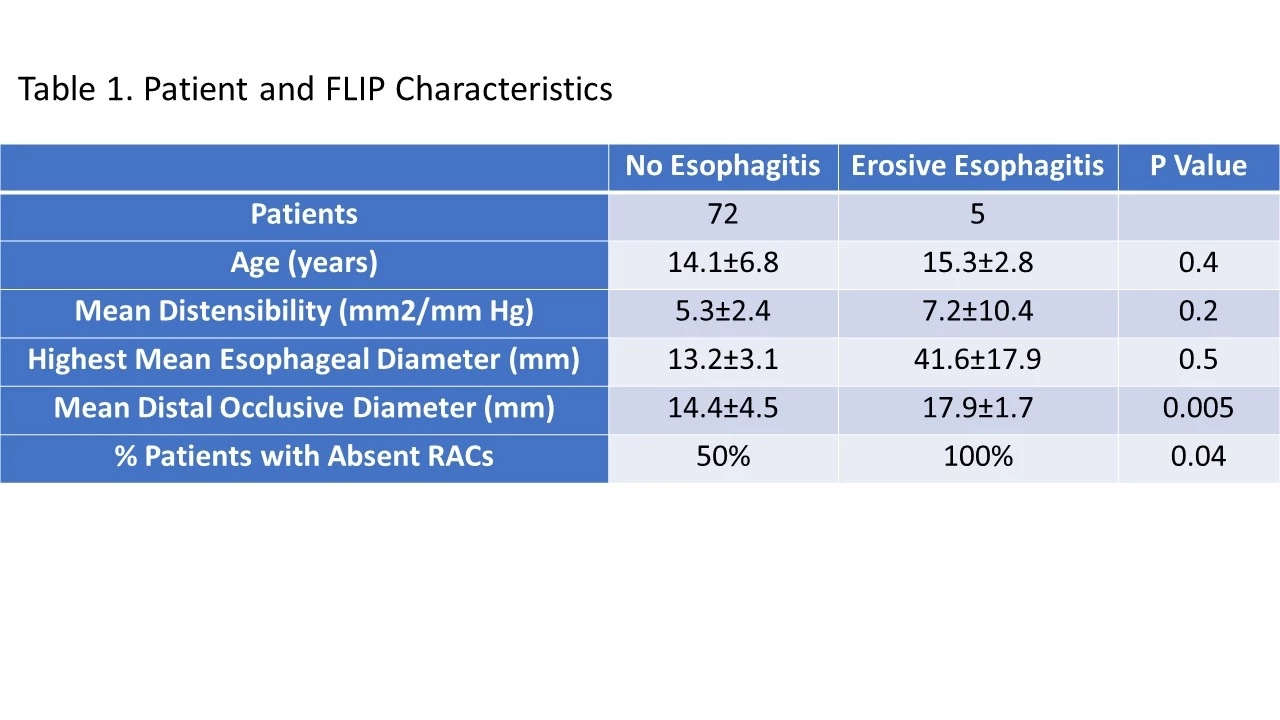
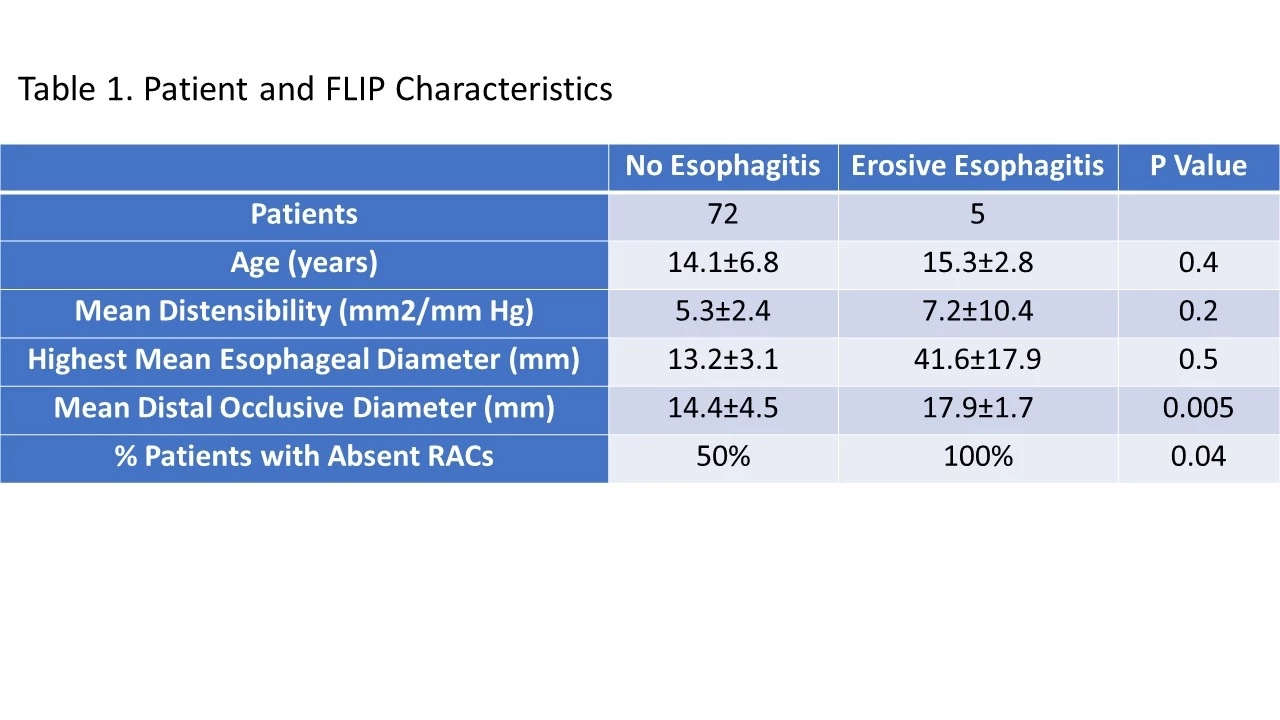
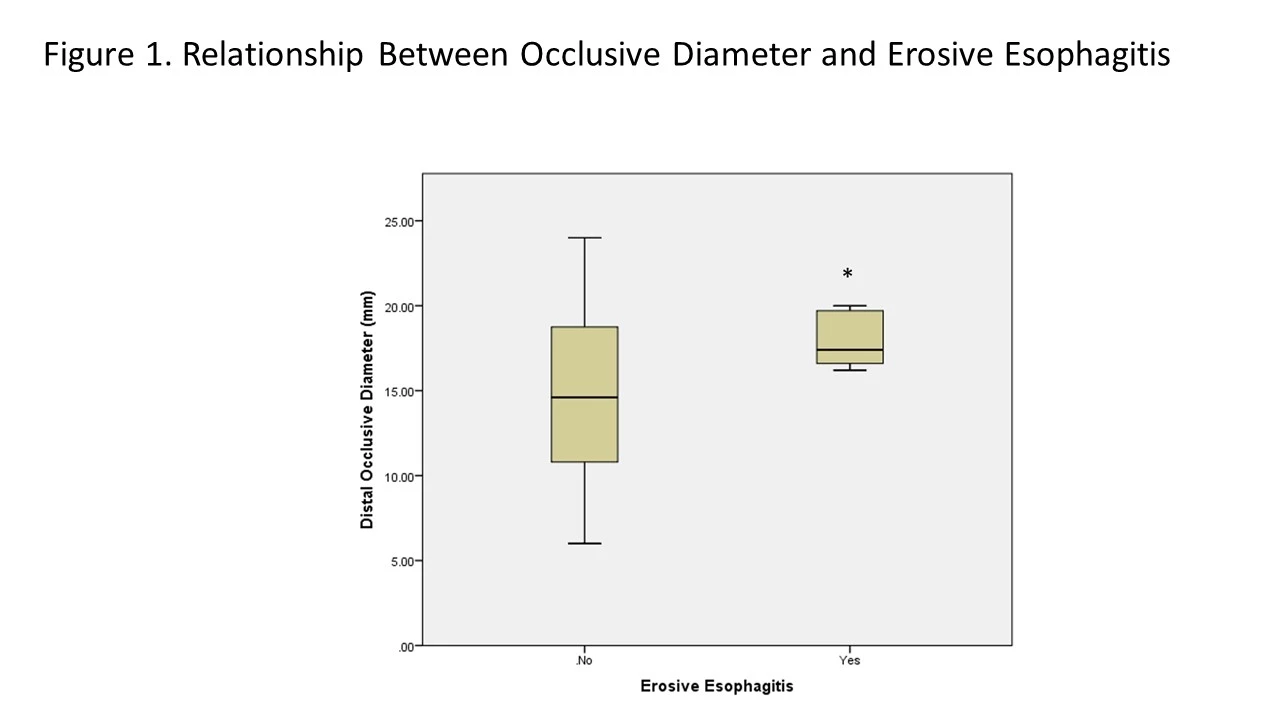
Background: Adult data suggests that disorders of primary peristalsis are associated with higher percent time pH<4 in the esophagus suggesting that abnormal peristalsis is associated with poor acid clearance. There are no studies of secondary peristalsis and its relationship to microscopic or gross esophagitis. The goal of this study was to determine the relationship between functional luminal impaging probe (FLIP) parameters and the presence or absence of esophagitis.
Methods: We reviewed the esophageal biopsies and FLIP 2.0 tracings for 72 patients and each FLIP tracing was measured for esophagogastric junction (EGJ) distensibility, repetitive antegrade contractions presence, occlusive diameters, and repetitive antegrade contractions (RACs) frequency. These results were then compared between patients with and without microscopic esophagitis and with and without erosive esophagitis. Means were compared using t tests. Proportions were compared using Chi-Square analyses.
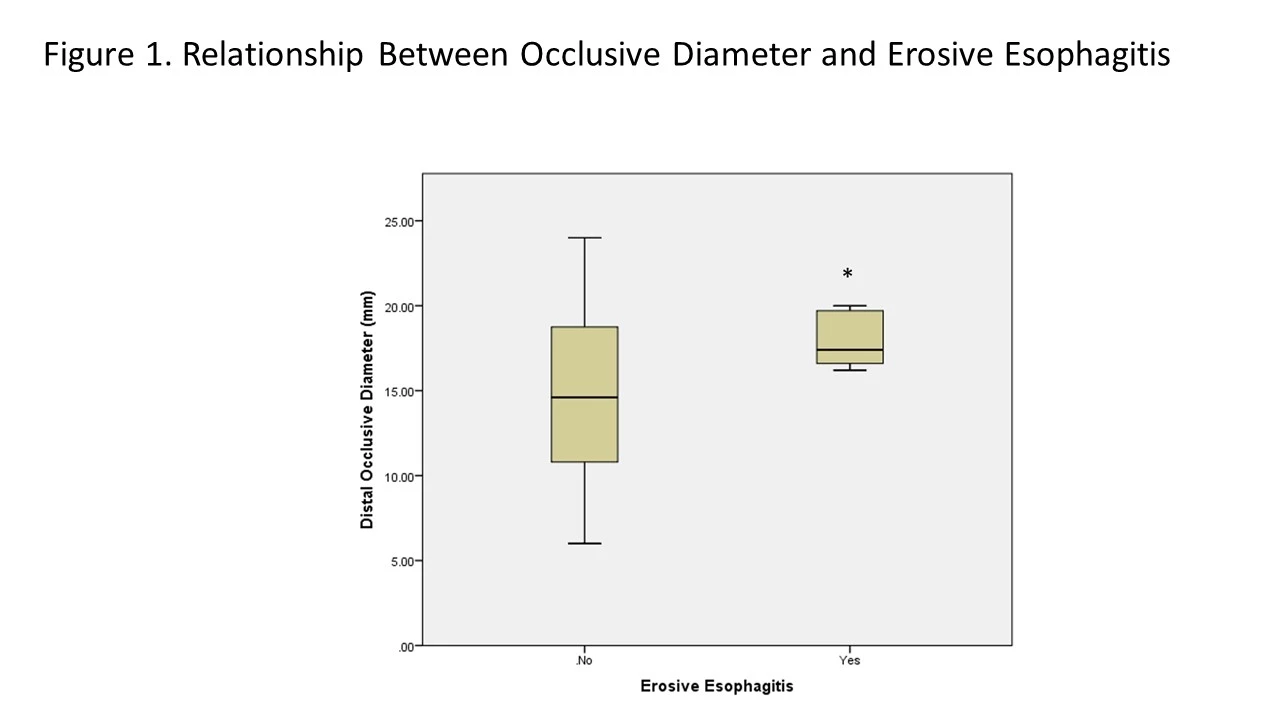
Results: 72 patients were included in the analysis. The mean age of patients was 14.2 + 6.5 years. Five (6.9%) patients had erosive esophagitis and 26 (36%) patients had microscopic esophagitis. Erosive esophagitis was strongly associated with disorders of secondary peristalsis as shown in the Table; in patients with erosive esophagitis, occlusive diameters were significantly higher than patients without erosive esophagitis signifying weaker peristalsis in patients with inflammation (Figure). When RAC presence and morphology was dichotomized into normal or abnormal RACs, there was a significant relationship between the presence of abnormal RACs and the presence of erosive esophagitis (p=0.04). In contrast, there was no relationship between any of the FLIP parameters and the presence of any microscopic esophagitis or the presence of > 15 eosinophils per high power field in the distal esophagus (p>0.3). There was no relationship of EGJ distensibility and the presence of erosive esophagitis or microscopic esophagitis (p>0.2).
Conclusions: Disorders of secondary peristalsis may be associated with erosive esophagitis, a relationship that is not seen with microscopic abnormalities. EGJ distensibility did not impact esophagitis risk.
Methods: We reviewed the esophageal biopsies and FLIP 2.0 tracings for 72 patients and each FLIP tracing was measured for esophagogastric junction (EGJ) distensibility, repetitive antegrade contractions presence, occlusive diameters, and repetitive antegrade contractions (RACs) frequency. These results were then compared between patients with and without microscopic esophagitis and with and without erosive esophagitis. Means were compared using t tests. Proportions were compared using Chi-Square analyses.
Results: 72 patients were included in the analysis. The mean age of patients was 14.2 + 6.5 years. Five (6.9%) patients had erosive esophagitis and 26 (36%) patients had microscopic esophagitis. Erosive esophagitis was strongly associated with disorders of secondary peristalsis as shown in the Table; in patients with erosive esophagitis, occlusive diameters were significantly higher than patients without erosive esophagitis signifying weaker peristalsis in patients with inflammation (Figure). When RAC presence and morphology was dichotomized into normal or abnormal RACs, there was a significant relationship between the presence of abnormal RACs and the presence of erosive esophagitis (p=0.04). In contrast, there was no relationship between any of the FLIP parameters and the presence of any microscopic esophagitis or the presence of > 15 eosinophils per high power field in the distal esophagus (p>0.3). There was no relationship of EGJ distensibility and the presence of erosive esophagitis or microscopic esophagitis (p>0.2).
Conclusions: Disorders of secondary peristalsis may be associated with erosive esophagitis, a relationship that is not seen with microscopic abnormalities. EGJ distensibility did not impact esophagitis risk.
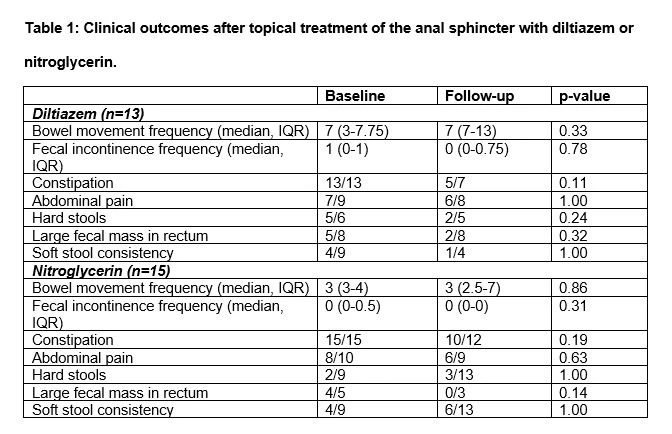
Background: Functional constipation (FC) in children often involves difficulty relaxing the anal sphincter or pelvic floor, and therefore topical treatment to allow relaxation of the anal sphincter may be beneficial. Our objective is to describe outcomes and safety of children with FC treated with topical treatment.
Methods: We performed a retrospective review of children with FC treated with topical treatment of the anal sphincter using topical diltiazem, nifedipine, or nitroglycerin at our institution. We recorded baseline demographics, medical history, symptoms at baseline and follow up, and any reported side effects.
Results: We identified 103 patients who were prescribed topical treatment of the anal sphincter at our institution and excluded 46 with an organic cause of constipation (38 with Hirschsprung disease, 5 anorectal malformation, 2 inflammatory bowel disease, 1 tethered spinal cord), 11 with anal fissure, 2 with internal anal sphincter achalasia, and 15 patients with FC without follow up data. We included 29 patients (59% female, median age 7 years, range 1-21) in our study. 13 patients were treated with diltiazem (61% male, median age 7 years, range 3-12). Diltiazem was applied 2 times a day (range 1-2) for a median of 3 months (range 2 weeks-1.5 years) at follow up. At follow up, 3 had stopped diltiazem: 1 because of lack of improvement, 1 because of patient refusal, 1 after anal sphincter botulinum toxin injection. 7/13 reported improvement: 3 in fecal incontinence, 2 in constipation, and 1 in abdominal pain. As shown in Table 1, presence of specific constipation symptoms did not change after treatment with diltiazem. 1/13 reported flatulence as a side effect. At follow up, 8/13 patients continued diltiazem treatment. Only 1 patient, an 11-year-old female, was treated with nifedipine. Nifedipine was applied 2 times a day for 1 month before stopping because of lack of improvement. 15 patients were treated with nitroglycerin (73% female, median age 8 years, range 1-21). Nitroglycerin was applied 2 times a day (range 1-2) for a median of 1.5 months (range 1 week-12 months) at follow up. At follow up, 5 had stopped nitroglycerin: 3 because of side effects, 1 because of lack of improvement, 1 for unclear reasons. 4/15 reported improvement: 3 in abdominal pain and 2 in constipation. Presence of specific constipation symptoms did not change after treatment. 4/15 patients experienced side effects: rash (1), discoloration of anus (1), and burning sensation (1). At follow up, 3/15 patients continued nitroglycerin treatment.
Discussion: In the first study of topical treatment of the anal sphincter for children with functional constipation, we found that diltiazem and nitroglycerin were generally well-tolerated with only minor side effects reported. Up to half of children treated with these topical treatments reported benefit.
Methods: We performed a retrospective review of children with FC treated with topical treatment of the anal sphincter using topical diltiazem, nifedipine, or nitroglycerin at our institution. We recorded baseline demographics, medical history, symptoms at baseline and follow up, and any reported side effects.
Results: We identified 103 patients who were prescribed topical treatment of the anal sphincter at our institution and excluded 46 with an organic cause of constipation (38 with Hirschsprung disease, 5 anorectal malformation, 2 inflammatory bowel disease, 1 tethered spinal cord), 11 with anal fissure, 2 with internal anal sphincter achalasia, and 15 patients with FC without follow up data. We included 29 patients (59% female, median age 7 years, range 1-21) in our study. 13 patients were treated with diltiazem (61% male, median age 7 years, range 3-12). Diltiazem was applied 2 times a day (range 1-2) for a median of 3 months (range 2 weeks-1.5 years) at follow up. At follow up, 3 had stopped diltiazem: 1 because of lack of improvement, 1 because of patient refusal, 1 after anal sphincter botulinum toxin injection. 7/13 reported improvement: 3 in fecal incontinence, 2 in constipation, and 1 in abdominal pain. As shown in Table 1, presence of specific constipation symptoms did not change after treatment with diltiazem. 1/13 reported flatulence as a side effect. At follow up, 8/13 patients continued diltiazem treatment. Only 1 patient, an 11-year-old female, was treated with nifedipine. Nifedipine was applied 2 times a day for 1 month before stopping because of lack of improvement. 15 patients were treated with nitroglycerin (73% female, median age 8 years, range 1-21). Nitroglycerin was applied 2 times a day (range 1-2) for a median of 1.5 months (range 1 week-12 months) at follow up. At follow up, 5 had stopped nitroglycerin: 3 because of side effects, 1 because of lack of improvement, 1 for unclear reasons. 4/15 reported improvement: 3 in abdominal pain and 2 in constipation. Presence of specific constipation symptoms did not change after treatment. 4/15 patients experienced side effects: rash (1), discoloration of anus (1), and burning sensation (1). At follow up, 3/15 patients continued nitroglycerin treatment.
Discussion: In the first study of topical treatment of the anal sphincter for children with functional constipation, we found that diltiazem and nitroglycerin were generally well-tolerated with only minor side effects reported. Up to half of children treated with these topical treatments reported benefit.
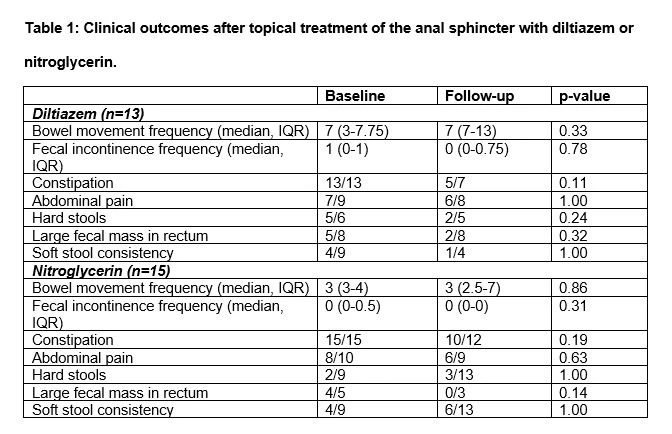
Table 1: Clinical outcomes after topical treatment of the anal sphincter with diltiazem or nitroglycerin.
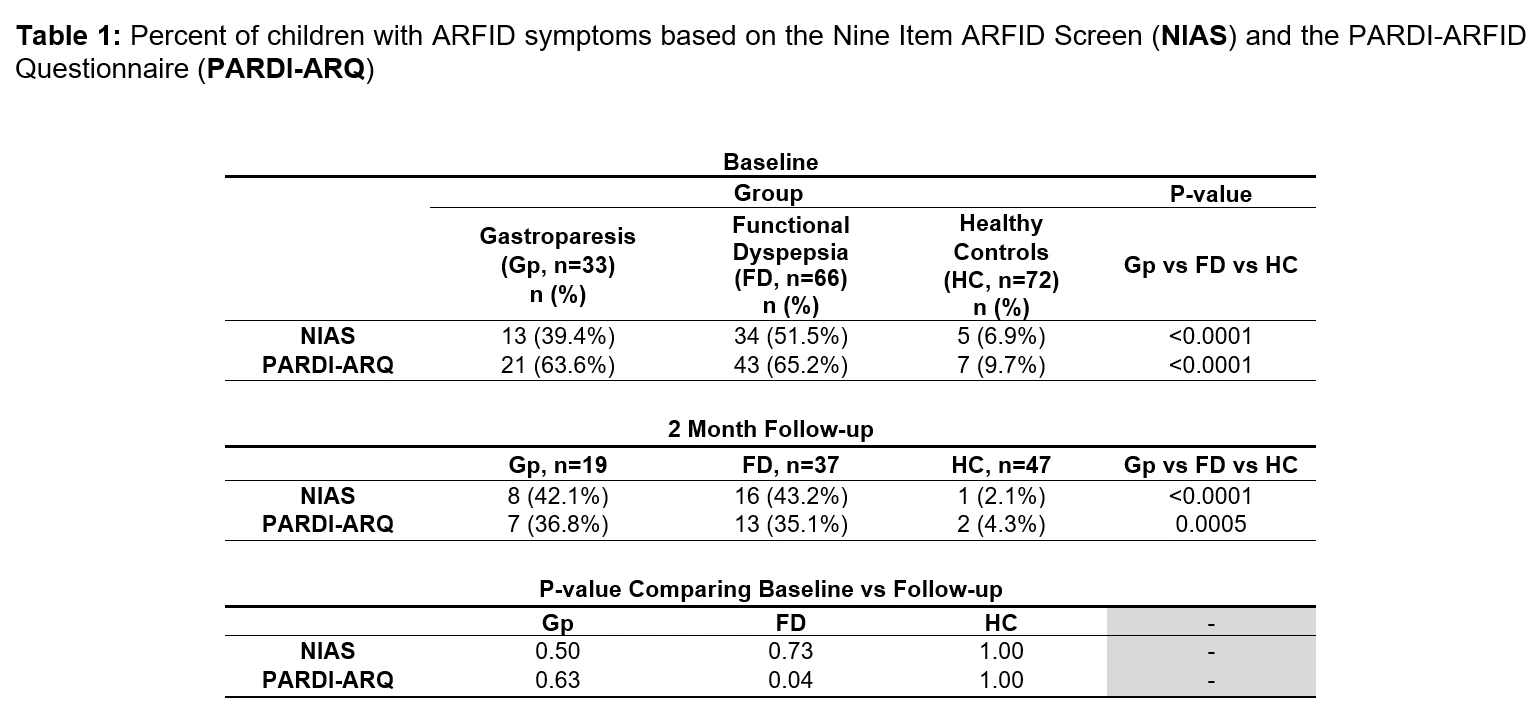
Background: Avoidant/restrictive food intake disorder (ARFID) occurs in up to 40% of adults with gastroparesis (Gp) and/or functional dyspepsia (FD); however, the prevalence among children with Gp and FD is unclear, particularly in relation to healthy children (HC).
Our Aims were to identify the prevalence of ARFID based on symptoms and its trajectory over two months in a longitudinal study in children with Gp, FD, and in HC.
Methods: Patients ages 10-17 years diagnosed with Gp or FD (based on abnormal/normal 4-hour gastric emptying scintigraphy, respectively, and presence of dyspeptic symptoms) and age- and sex-matched HC (no gastrointestinal complaints) completed two questionnaires to identify ARFID based on symptoms: the Nine Item ARFID Screen (NIAS) and the Pica ARFID Rumination Disorder Interview-ARFID Questionnaire (PARDI-ARQ). The questionnaires were readministered 2 months later. Criteria for identifying ARFID symptoms were based on previously published cutoff values (NIAS, PMID: 32677153; PARDI-ARQ, PMID:36419081).
Results: Median age at baseline was 15 years (range: 10-17) with no significant difference among the Gp (n=33), FD (n=66), or HC (n=72) groups. There were no significant differences among groups based on gender or ethnicity. A lower proportion of participants identified as Black in the Gp (15%) and FD (11%) groups than in the HC (36%) (P<0.01).
At baseline, the proportion of individuals with ARFID symptoms based on the NIAS was highest in the FD group (51.5%), followed by the Gp (39.4%) and HC groups (6.9%) (Table 1). Similarly, the proportion based on PARDI-ARQ was highest in the FD group (65.2%), followed by the Gp (63.6%) and HC groups (9.7%) (Table 1). A higher proportion of children were identified as having ARFID symptoms by PARDI-ARQ (P<0.001).
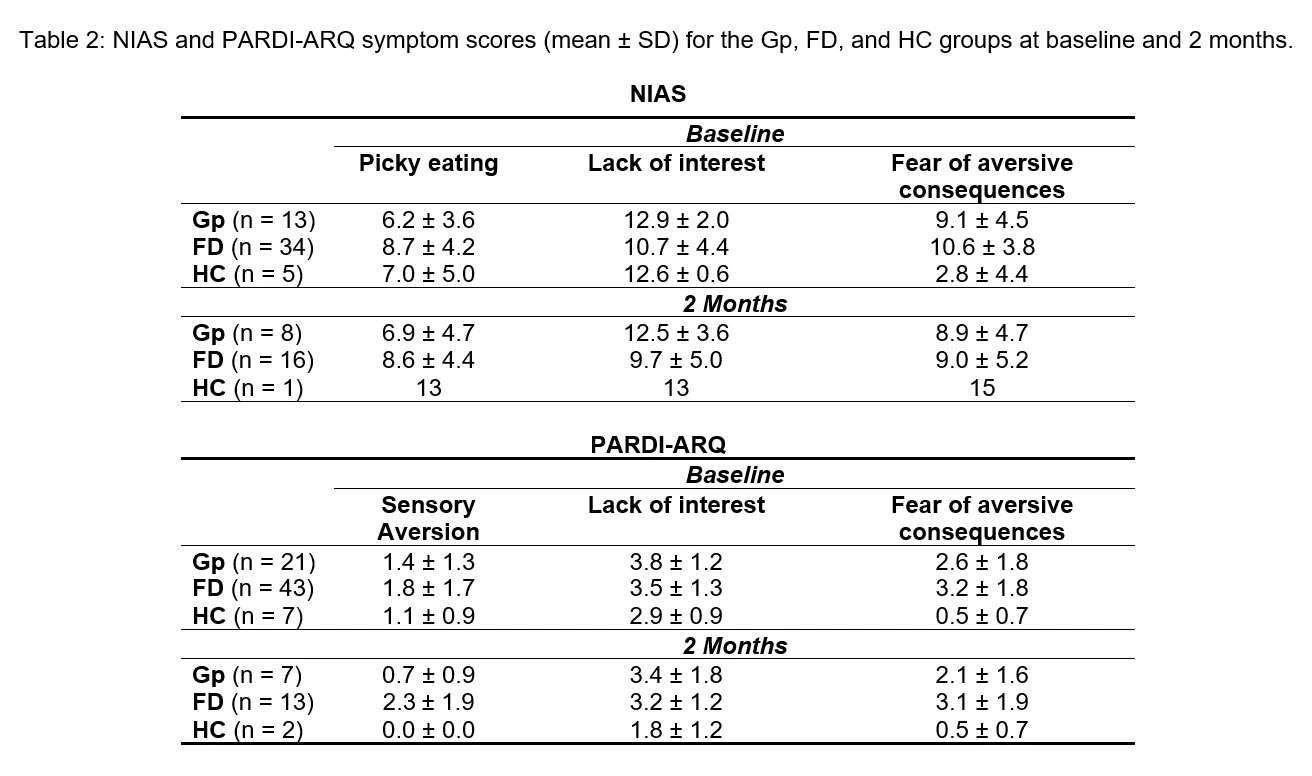
At 2 months, the overall proportion of children with ARFID symptoms in the Gp and FD groups did not change based on the NIAS but was lower in the FD group based on PARDI-ARQ (P=0.04, Table 1). Of the 52 children with ARFID symptoms at baseline based on the NIAS, 48% (25/52) completed the questionnaire at 2 months. Of these 25 children, 75% (6/8) of those with Gp and 69% (11/16) of those with FD continued to have ARFID symptoms at 2 months; the one HC child with ARFID symptoms at 2 months did not have ARFID at baseline. The most severe ARFID symptom at baseline and 2 months was ‘lack of interest’’ in eating (Table 2); however, “picky eating” was more severe in FD compared to Gp (baseline P=0.02; 2 months P=0.05).
Conclusions: ARFID symptoms are highly prevalent among children with Gp and FD but even can be identified in a small percentage of HC. Symptoms appear to persist for at least 2 months in a substantial proportion of children with Gp and FD. A ‘lack of interest’ in eating appears to be the most severe symptom. The ARFID questionnaire used can impact the prevalence of the diagnosis.
Our Aims were to identify the prevalence of ARFID based on symptoms and its trajectory over two months in a longitudinal study in children with Gp, FD, and in HC.
Methods: Patients ages 10-17 years diagnosed with Gp or FD (based on abnormal/normal 4-hour gastric emptying scintigraphy, respectively, and presence of dyspeptic symptoms) and age- and sex-matched HC (no gastrointestinal complaints) completed two questionnaires to identify ARFID based on symptoms: the Nine Item ARFID Screen (NIAS) and the Pica ARFID Rumination Disorder Interview-ARFID Questionnaire (PARDI-ARQ). The questionnaires were readministered 2 months later. Criteria for identifying ARFID symptoms were based on previously published cutoff values (NIAS, PMID: 32677153; PARDI-ARQ, PMID:36419081).
Results: Median age at baseline was 15 years (range: 10-17) with no significant difference among the Gp (n=33), FD (n=66), or HC (n=72) groups. There were no significant differences among groups based on gender or ethnicity. A lower proportion of participants identified as Black in the Gp (15%) and FD (11%) groups than in the HC (36%) (P<0.01).
At baseline, the proportion of individuals with ARFID symptoms based on the NIAS was highest in the FD group (51.5%), followed by the Gp (39.4%) and HC groups (6.9%) (Table 1). Similarly, the proportion based on PARDI-ARQ was highest in the FD group (65.2%), followed by the Gp (63.6%) and HC groups (9.7%) (Table 1). A higher proportion of children were identified as having ARFID symptoms by PARDI-ARQ (P<0.001).
At 2 months, the overall proportion of children with ARFID symptoms in the Gp and FD groups did not change based on the NIAS but was lower in the FD group based on PARDI-ARQ (P=0.04, Table 1). Of the 52 children with ARFID symptoms at baseline based on the NIAS, 48% (25/52) completed the questionnaire at 2 months. Of these 25 children, 75% (6/8) of those with Gp and 69% (11/16) of those with FD continued to have ARFID symptoms at 2 months; the one HC child with ARFID symptoms at 2 months did not have ARFID at baseline. The most severe ARFID symptom at baseline and 2 months was ‘lack of interest’’ in eating (Table 2); however, “picky eating” was more severe in FD compared to Gp (baseline P=0.02; 2 months P=0.05).
Conclusions: ARFID symptoms are highly prevalent among children with Gp and FD but even can be identified in a small percentage of HC. Symptoms appear to persist for at least 2 months in a substantial proportion of children with Gp and FD. A ‘lack of interest’ in eating appears to be the most severe symptom. The ARFID questionnaire used can impact the prevalence of the diagnosis.
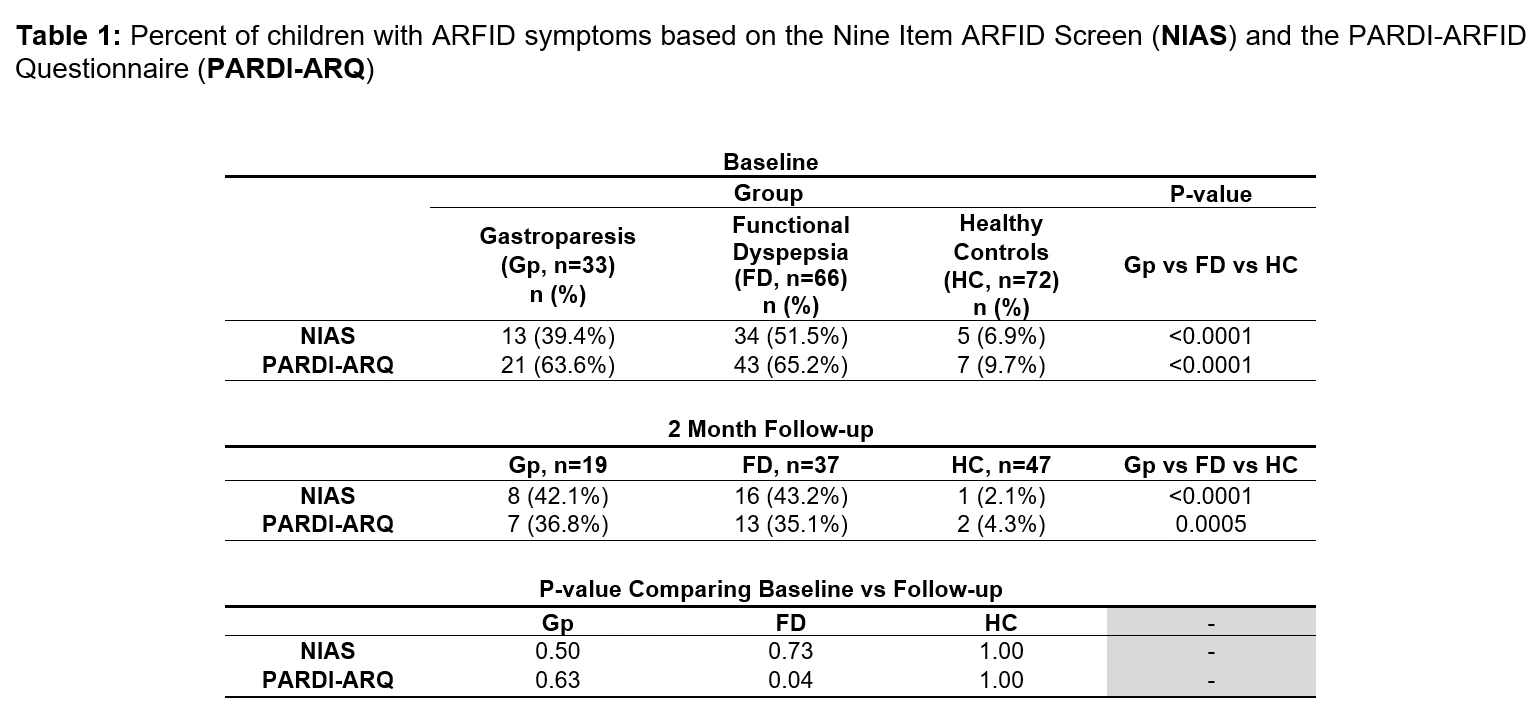
Table 1: Percent of children with ARFID symptoms based on the Nine Item ARFID Screen (NIAS) and the PARDI-ARFID Questionnaire (PARDI-ARQ)
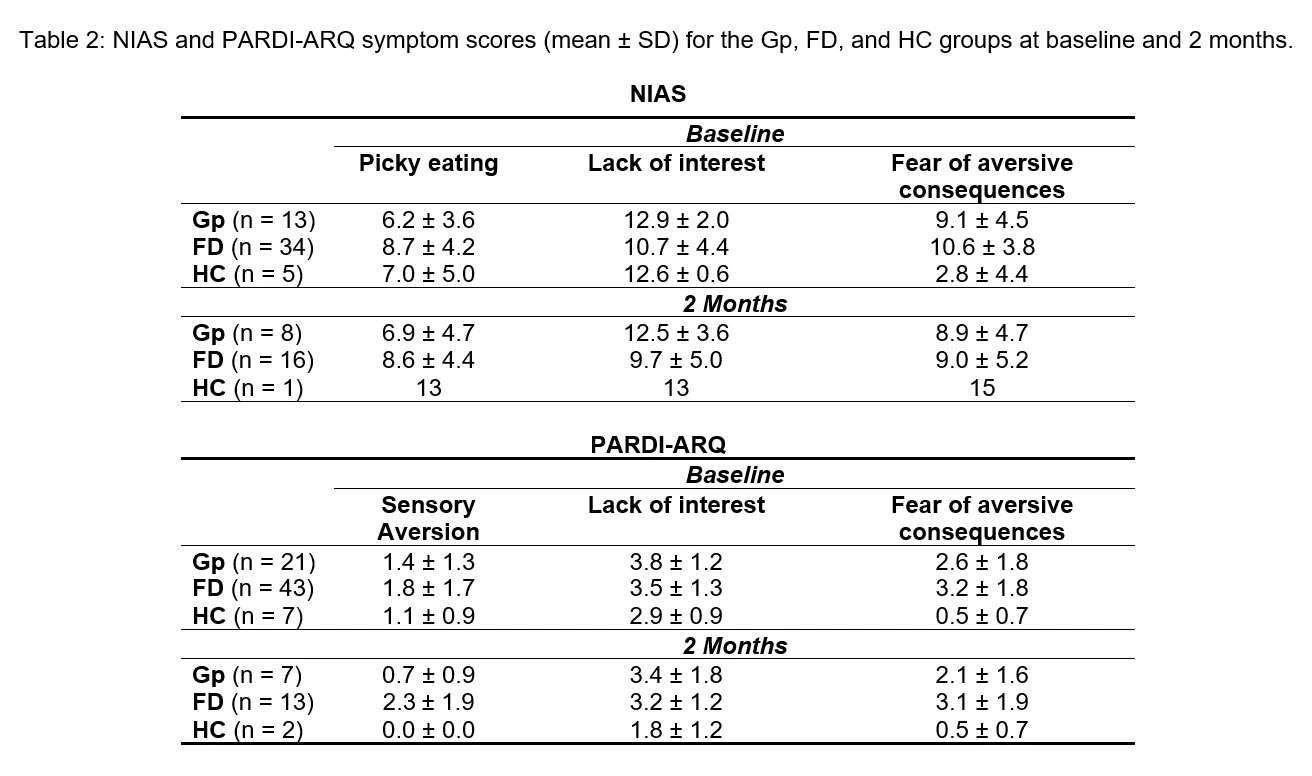
Table 2: NIAS and PARDI-ARQ symptom scores (mean ± SD) for the Gp, FD, and HC groups at baseline and 2 months.
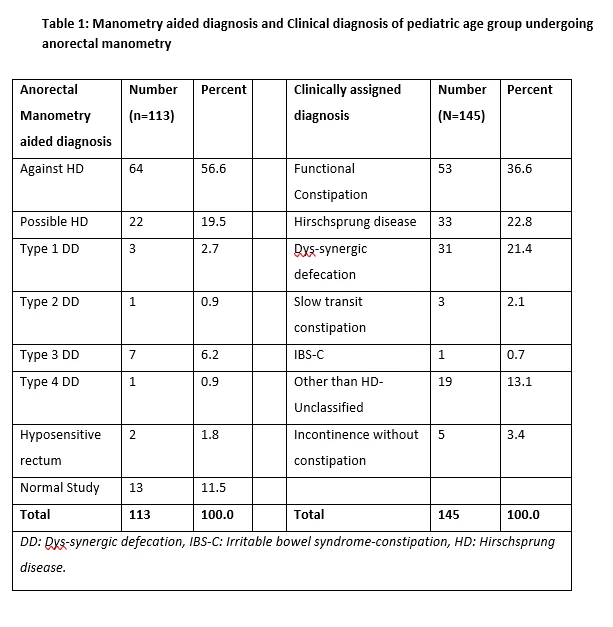
Introduction: Altered defecation patterns are common in childhood. Hirschsprung disease (HD) and non-HD phenotypes have different prognostic implications. Early childhood intestinal surgeries require anal sphincter assessment to decide re-closure of stoma. Anorectal manometry plays a key role in both clinical situations.
Methods: Retrospective data was retrieved from a prospectively maintained motility laboratory database from July 2008 to June 2022 to identify consecutive children between 0-18 years with defecation disorders undergoing anorectal manometry (ARM). Clinical history, contrast enema, flexible sigmoidoscopy when done, and ARM findings noted. Manometry performed using 20 channel water perfusion system from July 2008 to June 2017 and 20 channel solid state system from July 2017 till June 2022 (Medical Measurement Systems v 9.5i and 9.6d respectively). Two independent observers analyzed the clinical and manometric data respectively.
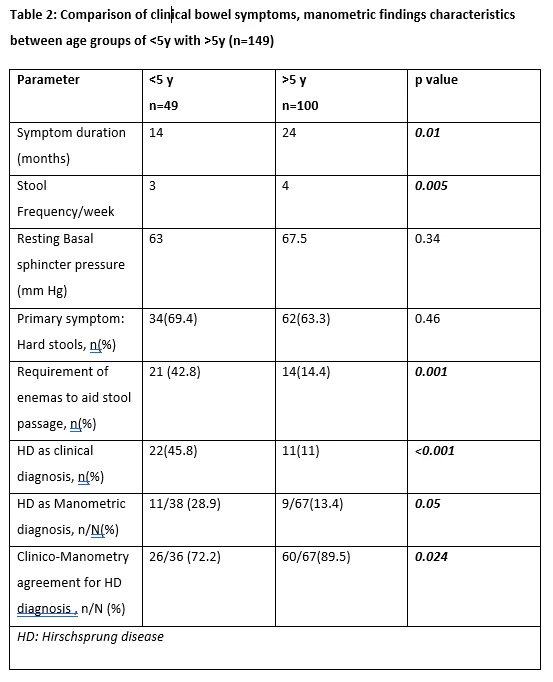
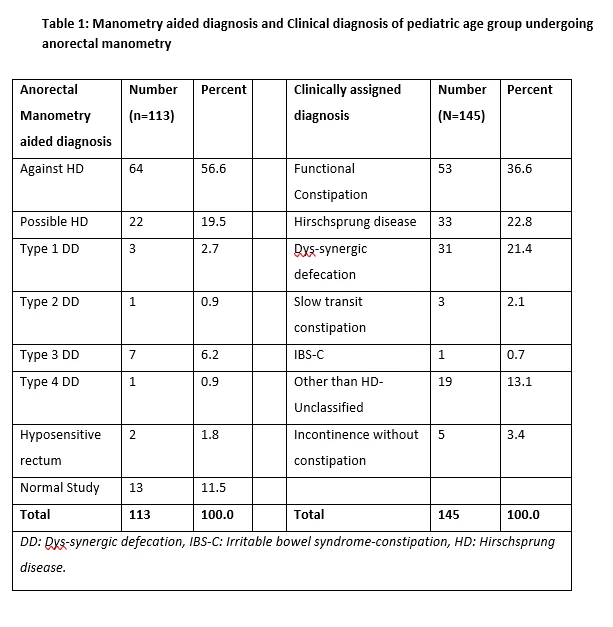
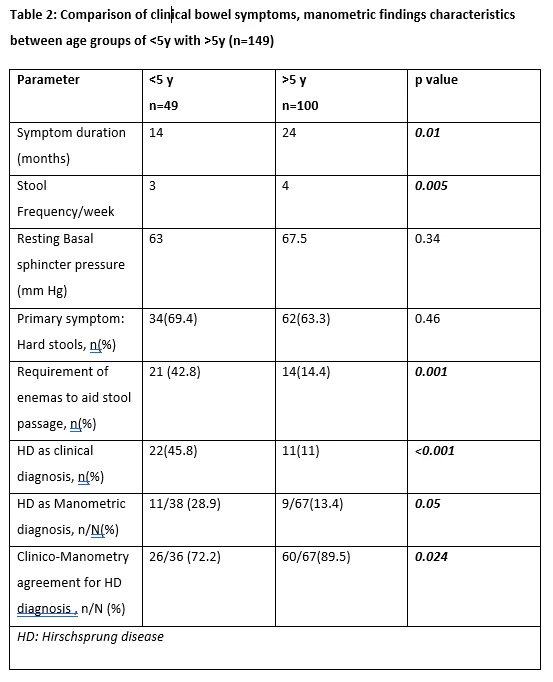
Results: One hundred and sixty children[64.4% males, median(IQR) age 84(36-180) mo, weight 18(10-40) Kg and symptom duration of 18(6-48)mo] underwent anorectal manometry over the specified duration. 113 patients assigned a best possible manometric diagnosis, and 145 classified into a best possible clinical diagnosis (table 1). The three most common symptom codes for which anorectal manometry was performed were: Hard stools with or without poor frequency (≤2/week, in >4 y age) 33.6%, incomplete evacuation or prolonged straining 22.6%, and fecal incontinence 11.6%. ARM as a tool for assessing sphincter function to establish closure of colostomy or ileostomy in children with previous surgery constituted 8.2% of all indications. Physician decision making was influenced in 42% cases with advice regarding pelvic muscle or sphincter strengthening exercises. Clinical diagnosis of Hirschsprung disease was made significantly more in <5y age than in >5y (p<0.001), and similarly manometric findings supportive of HD was seen more frequently in <5y age (p=0.05) (table2). Balloon expulsion test could be performed in 34% among >5y and only 4% of those<5y (p<0.001). Agreement between clinico-radiologic and manometric diagnosis for Hirschsprung disease was seen in overall 83.48%, with Cohen’s kappa statistic of 0.488 (moderate agreement, p<0.001) being higher in >5y group (89.5% vs 72.2% in<5y, p=0.024). Among 16.5% cases with disagreement, clinical diagnosis favored in 5%, manometric diagnosis favored in 11% and further evaluation done in 84%.
Conclusions: Constipation subtypes can be distinguished with help of ARM in pediatric population, effectively across ages. ARM influences physician planned decision on establishment of gut continuity in nearly half cases. There is moderate agreement between clinical assessment and manometry assisted diagnosis in discriminating organic from functional constipation, more so in older children.
Methods: Retrospective data was retrieved from a prospectively maintained motility laboratory database from July 2008 to June 2022 to identify consecutive children between 0-18 years with defecation disorders undergoing anorectal manometry (ARM). Clinical history, contrast enema, flexible sigmoidoscopy when done, and ARM findings noted. Manometry performed using 20 channel water perfusion system from July 2008 to June 2017 and 20 channel solid state system from July 2017 till June 2022 (Medical Measurement Systems v 9.5i and 9.6d respectively). Two independent observers analyzed the clinical and manometric data respectively.
Results: One hundred and sixty children[64.4% males, median(IQR) age 84(36-180) mo, weight 18(10-40) Kg and symptom duration of 18(6-48)mo] underwent anorectal manometry over the specified duration. 113 patients assigned a best possible manometric diagnosis, and 145 classified into a best possible clinical diagnosis (table 1). The three most common symptom codes for which anorectal manometry was performed were: Hard stools with or without poor frequency (≤2/week, in >4 y age) 33.6%, incomplete evacuation or prolonged straining 22.6%, and fecal incontinence 11.6%. ARM as a tool for assessing sphincter function to establish closure of colostomy or ileostomy in children with previous surgery constituted 8.2% of all indications. Physician decision making was influenced in 42% cases with advice regarding pelvic muscle or sphincter strengthening exercises. Clinical diagnosis of Hirschsprung disease was made significantly more in <5y age than in >5y (p<0.001), and similarly manometric findings supportive of HD was seen more frequently in <5y age (p=0.05) (table2). Balloon expulsion test could be performed in 34% among >5y and only 4% of those<5y (p<0.001). Agreement between clinico-radiologic and manometric diagnosis for Hirschsprung disease was seen in overall 83.48%, with Cohen’s kappa statistic of 0.488 (moderate agreement, p<0.001) being higher in >5y group (89.5% vs 72.2% in<5y, p=0.024). Among 16.5% cases with disagreement, clinical diagnosis favored in 5%, manometric diagnosis favored in 11% and further evaluation done in 84%.
Conclusions: Constipation subtypes can be distinguished with help of ARM in pediatric population, effectively across ages. ARM influences physician planned decision on establishment of gut continuity in nearly half cases. There is moderate agreement between clinical assessment and manometry assisted diagnosis in discriminating organic from functional constipation, more so in older children.
Tracks
Related Products
BASELINE AMMONIA LEVELS PREDICT MORTALITY AND LIVER-RELATED COMPLICATIONS IN ACUTE-ON-CHRONIC LIVER FAILURE PATIENTS
BACKGROUND: Hepatic encephalopathy (HE) is associated with increased mortality, falls, and frequent hospitalizations. Patient reported outcomes (PROs) are useful tools to assess health-related quality of life (HRQOL) measures such as impairment of sleep, cognition, or activity…
HABITUAL MEAT INTAKE IS ASSOCIATED WITH INCREASED RISK OF DISEASE FLARE IN ULCERATIVE COLITIS: INITIAL RESULTS FROM THE PREDICCT STUDY
Switching from originator to biosimilar infliximab (IFX) is effective and safe. However, data on multiple switching are scarce. The Edinburgh IBD unit has undertaken three switch programmes: (1) Remicade to CT-P13 (2016), (2) CT-P13 to SB2 (2020), and (3) SB2 to CT-P13 (2021)…
A PHASE 2, RANDOMIZED, DOUBLE-BLIND, PLACEBO-CONTROLLED TRIAL OF PRA023 AS INDUCTION THERAPY IN PATIENTS WITH MODERATELY TO SEVERELY ACTIVE ULCERATIVE COLITIS: ARTEMIS-UC, COHORT 1
Switching from originator to biosimilar infliximab (IFX) is effective and safe. However, data on multiple switching are scarce. The Edinburgh IBD unit has undertaken three switch programmes: (1) Remicade to CT-P13 (2016), (2) CT-P13 to SB2 (2020), and (3) SB2 to CT-P13 (2021)…
ENCAPSULATED MICROBIOTA TRANSPLANT THERAPY IMPROVES PARTIAL MAYO SCORES IN ULCERATIVE COLITIS AND INDUCES RAPID ENGRAFTMENT COMPARED TO PLACEBO CONTROL
Switching from originator to biosimilar infliximab (IFX) is effective and safe. However, data on multiple switching are scarce. The Edinburgh IBD unit has undertaken three switch programmes: (1) Remicade to CT-P13 (2016), (2) CT-P13 to SB2 (2020), and (3) SB2 to CT-P13 (2021)…


