Preferred
(EDT)
121 - INTESTINAL MICROBIOME INFLUENCES SEVERITY OF RESPIRATORY VIRAL INFECTION VIA IMPACTING ALVEOLAR MACROPHAGES
11:24 AM - 11:36 AM EDT
Saturday, May 6, 2023Room: S105a (McCormick Place)Overview
Society: AGA
Background: Emerging evidence suggest that gut microbiota influence human health such as digestive functions and risk of sepsis. We hypothesize that using a novel oral microbiome formula (SIM01) can restore dysbiosis and reduce adverse clinical events among vulnerable individuals after COVID-19 vaccination.
Methods: In a single center, double-blind, randomized, parallel arm, placebo-controlled trial, we recruited COVID-19 vaccination-naïve subjects (elderlies aged ≥ 65 years and patients with type 2 diabetes). After receiving the first dose of COVID-19 vaccine (CoronaVac or BioNTech), eligible subjects were randomized in a 1:1 ratio to receive 3 months of SIM01 (containing 20 billion CFU of probiotics per day) or placebo (2 mg of vitamin C per day). Intervention (SIM01 or placebo) was initiated within 1 week of receiving COVID-19 vaccines to minimize confounding effects of COVID-19 infection. Follow-up assessments were arranged at 1 month and 3 months after second vaccine dose. Outcomes included (1) Adverse events (AEs), defined as new symptoms/diseases which exerted unfavourable impacts on subjects; and (2) Restoration of gut dysbiosis, defined as improvement in (i) gut microbiome composition and diversity; (ii) functional potential (i.e., MetaCyc pathway abundances); and (iii) proliferation of beneficial bacteria genus (i.e., bifidobacteria, eubacterium, roseburia and other short-chain fatty acids producers). Fecal microbiome analysis using shotgun metagenomic sequencing were performed at baseline and after 3 months. The study is registered in a clinical trial registry (NCT04884776).
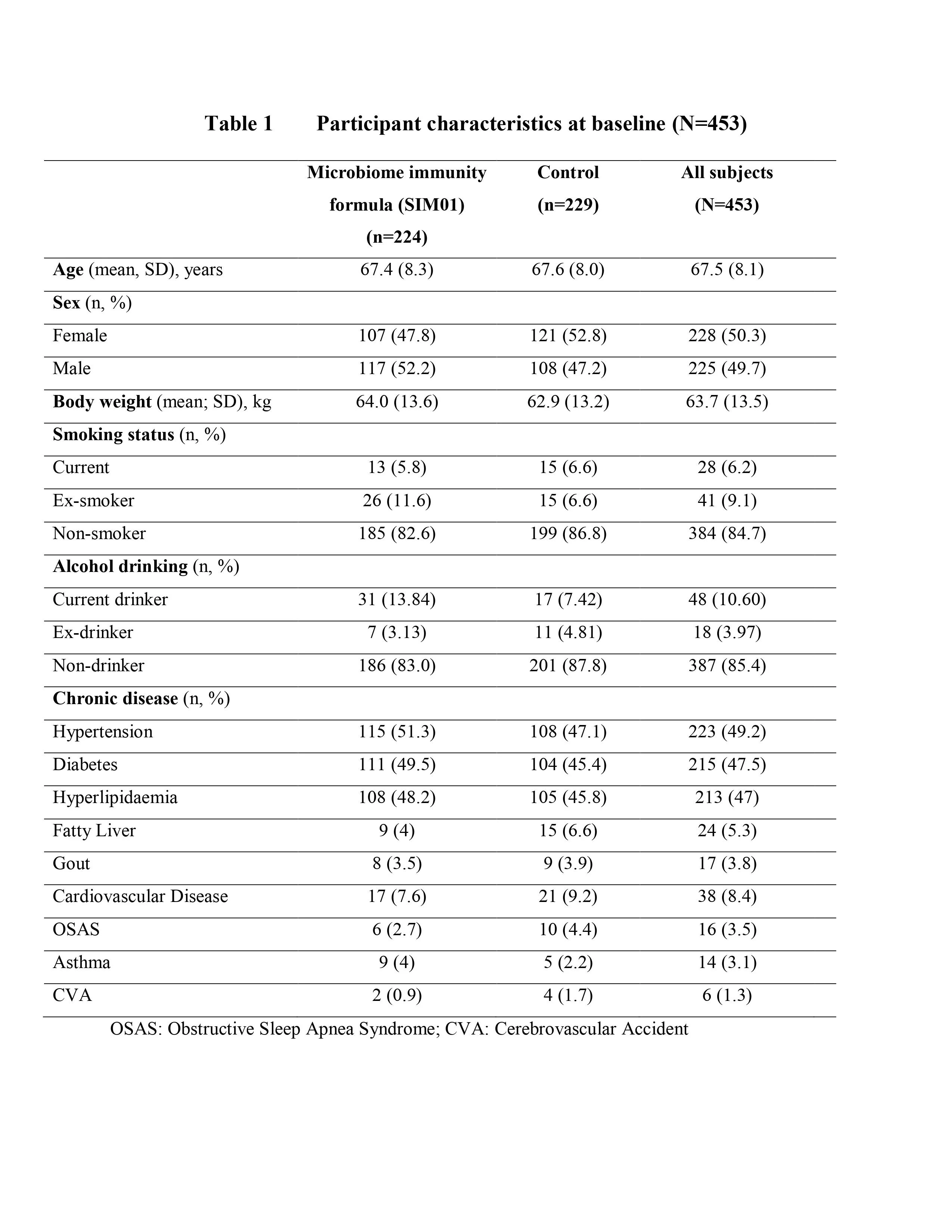
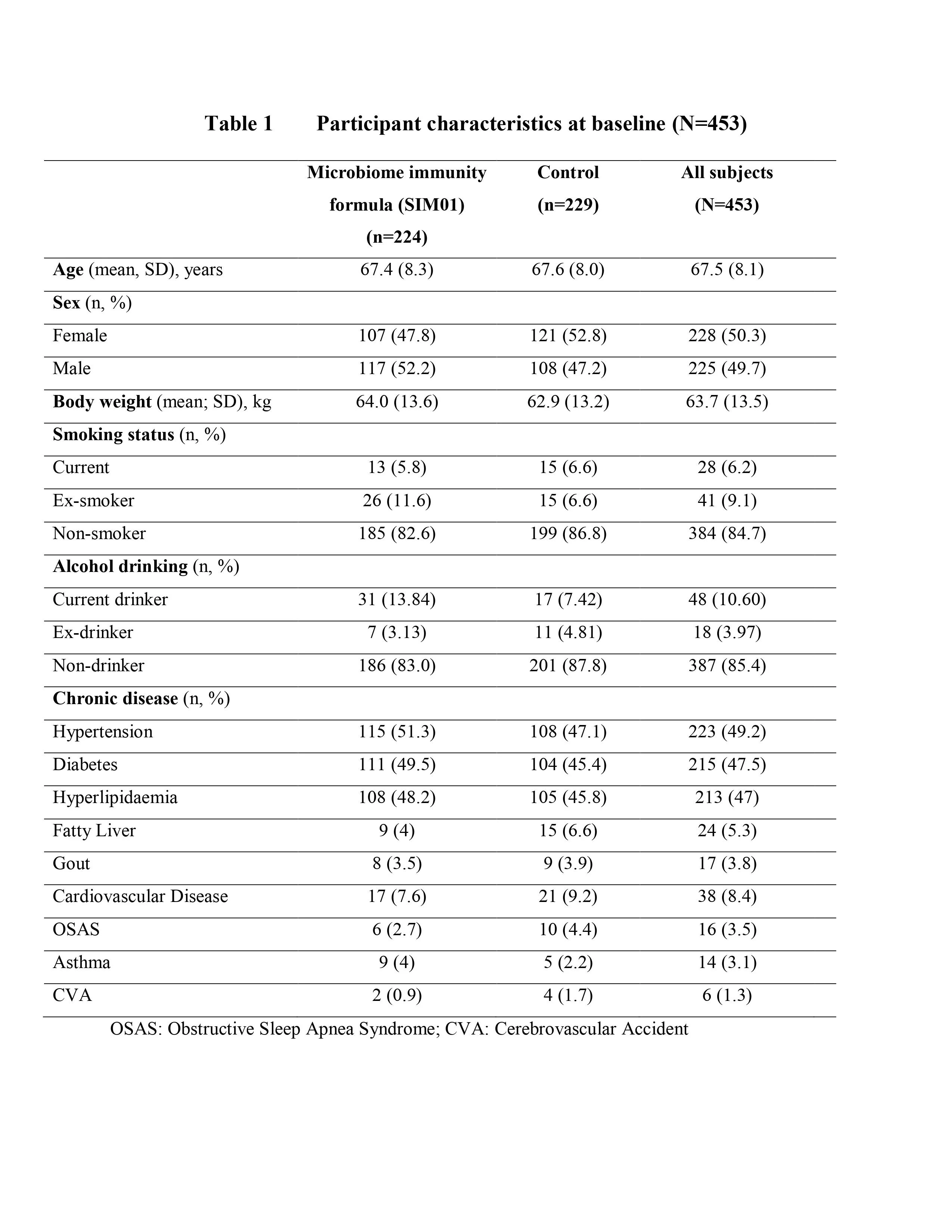
Results: Between April 2021 and March 2022, of 497 subjects assessed for eligibility, we recruited 453 individuals (50.3% females; mean age 67.5 years). We randomly assigned 224 subjects to SIM01 and 229 to placebo. There was no difference in baseline characteristics between the two groups (Table 1). The incidence of AE (2.9% vs. 10.6%, p=0.002) and combined AE/serious AE (2.9% vs. 12.6%, p<0.001) were significantly lower in SIM01 group than placebo group at 1 month. Rates of AE (0% vs. 2.5%, p=0.053) and combined AE/serious AE (0% vs. 3.1%, p=0.025) remained significantly lower in SIM01 than placebo group at 3 months. Overall, 70.4%, 18.5%, and 11.1% of the AEs and serious AEs at 1 month included gastrointestinal disturbance, dermatological conditions and infections, respectively. Probiotics in SIM01 successfully colonized in the gut. SIM01, but not placebo, led to a significant increase in beneficial bacteria and butyrate producers in fecal samples, enterotype shift from bacteroides to bifidobacteria and a strengthened microbial ecology network at 3 months after second vaccine dose.
Conclusion: SIM01 restored gut dysbiosis, reduced adverse clinical outcomes and strengthened gut microbiome resilience in elderly people and diabetes patients after COVID-19 vaccination.
Methods: In a single center, double-blind, randomized, parallel arm, placebo-controlled trial, we recruited COVID-19 vaccination-naïve subjects (elderlies aged ≥ 65 years and patients with type 2 diabetes). After receiving the first dose of COVID-19 vaccine (CoronaVac or BioNTech), eligible subjects were randomized in a 1:1 ratio to receive 3 months of SIM01 (containing 20 billion CFU of probiotics per day) or placebo (2 mg of vitamin C per day). Intervention (SIM01 or placebo) was initiated within 1 week of receiving COVID-19 vaccines to minimize confounding effects of COVID-19 infection. Follow-up assessments were arranged at 1 month and 3 months after second vaccine dose. Outcomes included (1) Adverse events (AEs), defined as new symptoms/diseases which exerted unfavourable impacts on subjects; and (2) Restoration of gut dysbiosis, defined as improvement in (i) gut microbiome composition and diversity; (ii) functional potential (i.e., MetaCyc pathway abundances); and (iii) proliferation of beneficial bacteria genus (i.e., bifidobacteria, eubacterium, roseburia and other short-chain fatty acids producers). Fecal microbiome analysis using shotgun metagenomic sequencing were performed at baseline and after 3 months. The study is registered in a clinical trial registry (NCT04884776).
Results: Between April 2021 and March 2022, of 497 subjects assessed for eligibility, we recruited 453 individuals (50.3% females; mean age 67.5 years). We randomly assigned 224 subjects to SIM01 and 229 to placebo. There was no difference in baseline characteristics between the two groups (Table 1). The incidence of AE (2.9% vs. 10.6%, p=0.002) and combined AE/serious AE (2.9% vs. 12.6%, p<0.001) were significantly lower in SIM01 group than placebo group at 1 month. Rates of AE (0% vs. 2.5%, p=0.053) and combined AE/serious AE (0% vs. 3.1%, p=0.025) remained significantly lower in SIM01 than placebo group at 3 months. Overall, 70.4%, 18.5%, and 11.1% of the AEs and serious AEs at 1 month included gastrointestinal disturbance, dermatological conditions and infections, respectively. Probiotics in SIM01 successfully colonized in the gut. SIM01, but not placebo, led to a significant increase in beneficial bacteria and butyrate producers in fecal samples, enterotype shift from bacteroides to bifidobacteria and a strengthened microbial ecology network at 3 months after second vaccine dose.
Conclusion: SIM01 restored gut dysbiosis, reduced adverse clinical outcomes and strengthened gut microbiome resilience in elderly people and diabetes patients after COVID-19 vaccination.
Background: Roseburia intestinalis is an anaerobic bacterium that has been shown to prevent intestinal inflammation by producing metabolites. We aimed to study the role of R. intestinalis in regulating colorectal tumorigenesis and immunotherapy through its metabolites.
Methods: The abundance of R. intestinalis was evaluated in stool samples of human CRC patients (n=444) and healthy subjects (n=575). The carcinogenic and immunomodulatory effects of R. intestinalis were studied in ApcMin/+ and AOM-induced CRC mouse models. The metabolites produced by R. intestinalis were evaluated by untargeted metabolomic profiling and targeted gas chromatography-mass spectrometry (GC-MS). The bio-functions of R. intestinalis cultured medium and candidate metabolites were examined in CRC cell lines (HCT116, LoVo, SW480). The change of immune landscape was evaluated by multicolor flow cytometry and immunohistochemistry staining. The effects of R. intestinalis and its metabolites on anti-PD-1 efficacy were assessed in two syngeneic mouse models of CT26 (MSI-low) and MC38 (MSI-high).
Results: R. intestinalis was significantly depleted in stool samples of CRC patients compared to healthy controls (P<0.05). R. intestinalis administration significantly inhibited colorectal tumorigenesis by reducing tumor incidence, tumor number and tumor size in ApcMin/+ mice, and further confirmed in AOM-induced CRC mice. R. intestinalis restored gut barrier functions as indicated by improved intestinal permeability and enhanced tight junction proteins ZO-1 and Claudin-3. R. intestinalis produced the metabolite butyrate which was identified as a functional component based on the metabolomic profiling assay and bio-functional validation in CRC cell lines. R. intestinalis significantly activated cytotoxic CD8+ T cells in colonic tumors of AOM-induced CRC mice. This was confirmed in both MC38 and CT26 orthotopic mouse models that R. intestinalis and butyrate suppressed tumor growth by inducing cytotoxic Granzyme B+, IFN-γ+ and TNF-α+ CD8+ T cells. Moreover, R. intestinalis and butyrate significantly improved anti-PD-1 efficacy in MSI-low CT26 orthotopic mouse model. Mechanistically, butyrate binds to TLR5 receptor of CD8+ T cells to induce its activity through activating NF-κB signaling. TLR5 inhibitor TH1020 abolished the effects of butyrate on activating CD8+ T cells and inducing NF-κB signalling.
Conclusions: R. intestinalis protects against CRC by producing butyrate in mice. R. intestinalis derived butyrate improved anti-PD-1 efficacy in CRC by inducing the functional CD8+ T cells through binding to the receptor of CD8+ T cells to activate the NF-κB signalling. R. intestinalis is a potential novel adjuvant therapy to augment anti-PD-1 efficacy against CRC.
Methods: The abundance of R. intestinalis was evaluated in stool samples of human CRC patients (n=444) and healthy subjects (n=575). The carcinogenic and immunomodulatory effects of R. intestinalis were studied in ApcMin/+ and AOM-induced CRC mouse models. The metabolites produced by R. intestinalis were evaluated by untargeted metabolomic profiling and targeted gas chromatography-mass spectrometry (GC-MS). The bio-functions of R. intestinalis cultured medium and candidate metabolites were examined in CRC cell lines (HCT116, LoVo, SW480). The change of immune landscape was evaluated by multicolor flow cytometry and immunohistochemistry staining. The effects of R. intestinalis and its metabolites on anti-PD-1 efficacy were assessed in two syngeneic mouse models of CT26 (MSI-low) and MC38 (MSI-high).
Results: R. intestinalis was significantly depleted in stool samples of CRC patients compared to healthy controls (P<0.05). R. intestinalis administration significantly inhibited colorectal tumorigenesis by reducing tumor incidence, tumor number and tumor size in ApcMin/+ mice, and further confirmed in AOM-induced CRC mice. R. intestinalis restored gut barrier functions as indicated by improved intestinal permeability and enhanced tight junction proteins ZO-1 and Claudin-3. R. intestinalis produced the metabolite butyrate which was identified as a functional component based on the metabolomic profiling assay and bio-functional validation in CRC cell lines. R. intestinalis significantly activated cytotoxic CD8+ T cells in colonic tumors of AOM-induced CRC mice. This was confirmed in both MC38 and CT26 orthotopic mouse models that R. intestinalis and butyrate suppressed tumor growth by inducing cytotoxic Granzyme B+, IFN-γ+ and TNF-α+ CD8+ T cells. Moreover, R. intestinalis and butyrate significantly improved anti-PD-1 efficacy in MSI-low CT26 orthotopic mouse model. Mechanistically, butyrate binds to TLR5 receptor of CD8+ T cells to induce its activity through activating NF-κB signaling. TLR5 inhibitor TH1020 abolished the effects of butyrate on activating CD8+ T cells and inducing NF-κB signalling.
Conclusions: R. intestinalis protects against CRC by producing butyrate in mice. R. intestinalis derived butyrate improved anti-PD-1 efficacy in CRC by inducing the functional CD8+ T cells through binding to the receptor of CD8+ T cells to activate the NF-κB signalling. R. intestinalis is a potential novel adjuvant therapy to augment anti-PD-1 efficacy against CRC.
Background: The recently enhanced capacity to test individuals for respiratory viruses, such as influenza virus (IAV), respiratory syncytial virus (RSV), and SARS/Cov-2, has led to the appreciation that severities of respiratory viral infections (RVI) are highly heterogenous ranging from asymptomatic infection to severe lung pathology and/or death.
Aim: We sought to investigate the hypothesis that intestinal microbiota composition is one factor that might influence severity of RVI.
Approach: Mice born with differing microbiomes were acquired from different vivaria or by administering mice the commensal bacteria segmented filamentous bacteria (SFB), which is naturally present in some vivaria. Nasal administration of H1N1 influenza virus (IAV) or respiratory syncytial virus (RSV) served as models of RVI.
Results: We observed that colonization of the intestine by SFB, naturally acquired or exogenously administered, lastingly protected mice against influenza virus (IAV) challenge, assessed by viral titers or clinical-type indices. Such protection was independent of type I and III interferons and adaptive immunity, IL-17/IL-22, and Stat1 signaling. Instead, it is associated with, and required, maintenance of alveolar macrophages (AMs), which, in mice lacking SFB, were quickly depleted as pandemic IAV replicated, leaving lung epithelial cells unguarded and thus highly prone to infection. Transplant of AMs from SFB+ to SFB- mice recapitulated the AM-emboldened phenotype and protected mice against IAV infection.
Conclusions: Gut microbiota composition can have dramatic impacts on alveolar macrophage phenotype and, consequently, be a major determinant RVI outcomes.
Aim: We sought to investigate the hypothesis that intestinal microbiota composition is one factor that might influence severity of RVI.
Approach: Mice born with differing microbiomes were acquired from different vivaria or by administering mice the commensal bacteria segmented filamentous bacteria (SFB), which is naturally present in some vivaria. Nasal administration of H1N1 influenza virus (IAV) or respiratory syncytial virus (RSV) served as models of RVI.
Results: We observed that colonization of the intestine by SFB, naturally acquired or exogenously administered, lastingly protected mice against influenza virus (IAV) challenge, assessed by viral titers or clinical-type indices. Such protection was independent of type I and III interferons and adaptive immunity, IL-17/IL-22, and Stat1 signaling. Instead, it is associated with, and required, maintenance of alveolar macrophages (AMs), which, in mice lacking SFB, were quickly depleted as pandemic IAV replicated, leaving lung epithelial cells unguarded and thus highly prone to infection. Transplant of AMs from SFB+ to SFB- mice recapitulated the AM-emboldened phenotype and protected mice against IAV infection.
Conclusions: Gut microbiota composition can have dramatic impacts on alveolar macrophage phenotype and, consequently, be a major determinant RVI outcomes.
Presenter
Other
AGA


