Preferred
(EDT)
704 - METHANE MADNESS: EVALUATING THE PREVALENCE OF INTESTINAL METHANOGEN OVERGROWTH
10:24 AM - 10:36 AM EDT
Monday, May 20, 2024Room: 103AB (Walter E. Washington Convention Center)Overview
Background: Small Intestinal Bacterial Overgrowth (SIBO) is the presence of excessive microbes in the small intestine. Jejunal aspiration and culture is the gold standard for diagnosis however it is limited by several factors. Breath testing is an alternative mechanism for SIBO diagnosis. Based on the predominant gas, SIBO can be divided into hydrogen-producing (H-SIBO) or methane-producing (IMO, intestinal methanogen overgrowth). Per North American consensus criteria, a 20 ppm or more rise in hydrogen from baseline is consistent with H-SIBO and a methane level of 10 ppm or greater at any time is consistent with IMO. Differentiating between the two impacts clinical decision-making as IMO requires an alternative treatment regimen. Studies have reported the incidence of IMO ranging from 8.6 to 50.4%, with a majority reporting values between 15 to 25%. This study aims to assess the incidence and characteristics of intestinal methanogen overgrowth at a large tertiary institute in the Mid-Atlantic region.
Methods: This retrospective cohort analysis identified 1,447 patients who underwent breath testing between 2017 - 2023. All breath testing was completed in the motility lab with stringent pre-test preparation and intraprocedural monitoring. We examined the demographic and medical history of these patients (age, sex, BMI, ethnicity, abdominal surgeries, IBS, IBD, celiac disease and gastroparesis). We then performed an initial t-test analysis of baseline and peak methane breath test results.
Results: Of 1,447 patients who underwent SIBO testing, 995 (68.7%) were positive for IMO, with an average peak methane of 26.7, while 249 (17.2%) tested positive for H-SIBO. IMO was significantly more frequent when compared to H-SIBO. Demographic data is similar across all groups (Table 1). Within the IMO positive cohort, 357 (36%) patients were found to have an elevated peak methane in the range of 10-14ppm, 191 (19%) from 15-19ppm and 447 (45%) ≥20 ppm (Table 2). The majority of IMO positive patients had elevated methane at baseline (67.6%).
Conclusions: Our data shows an overwhelming number of positive IMO patients, which differs from previously reported prevalence of IMO. These patients had comparable demographic distribution and baseline methane elevation when compared to previous studies. Experts have debated what methane level constitutes a positive test. Prior studies have reported that using the North American consensus guidelines leads to greater rates of IMO diagnosis when compared to other criteria. While there is a broad range of IMO positivity rates in the literature, our study demonstrates an impressively high level of IMO predominance. Reevaluating criteria for IMO diagnosis should be considered. Additional research is needed to better elucidate the underlying demographic and comorbid contributors of IMO and provide evidence-based criteria for diagnosis.
Methods: This retrospective cohort analysis identified 1,447 patients who underwent breath testing between 2017 - 2023. All breath testing was completed in the motility lab with stringent pre-test preparation and intraprocedural monitoring. We examined the demographic and medical history of these patients (age, sex, BMI, ethnicity, abdominal surgeries, IBS, IBD, celiac disease and gastroparesis). We then performed an initial t-test analysis of baseline and peak methane breath test results.
Results: Of 1,447 patients who underwent SIBO testing, 995 (68.7%) were positive for IMO, with an average peak methane of 26.7, while 249 (17.2%) tested positive for H-SIBO. IMO was significantly more frequent when compared to H-SIBO. Demographic data is similar across all groups (Table 1). Within the IMO positive cohort, 357 (36%) patients were found to have an elevated peak methane in the range of 10-14ppm, 191 (19%) from 15-19ppm and 447 (45%) ≥20 ppm (Table 2). The majority of IMO positive patients had elevated methane at baseline (67.6%).
Conclusions: Our data shows an overwhelming number of positive IMO patients, which differs from previously reported prevalence of IMO. These patients had comparable demographic distribution and baseline methane elevation when compared to previous studies. Experts have debated what methane level constitutes a positive test. Prior studies have reported that using the North American consensus guidelines leads to greater rates of IMO diagnosis when compared to other criteria. While there is a broad range of IMO positivity rates in the literature, our study demonstrates an impressively high level of IMO predominance. Reevaluating criteria for IMO diagnosis should be considered. Additional research is needed to better elucidate the underlying demographic and comorbid contributors of IMO and provide evidence-based criteria for diagnosis.
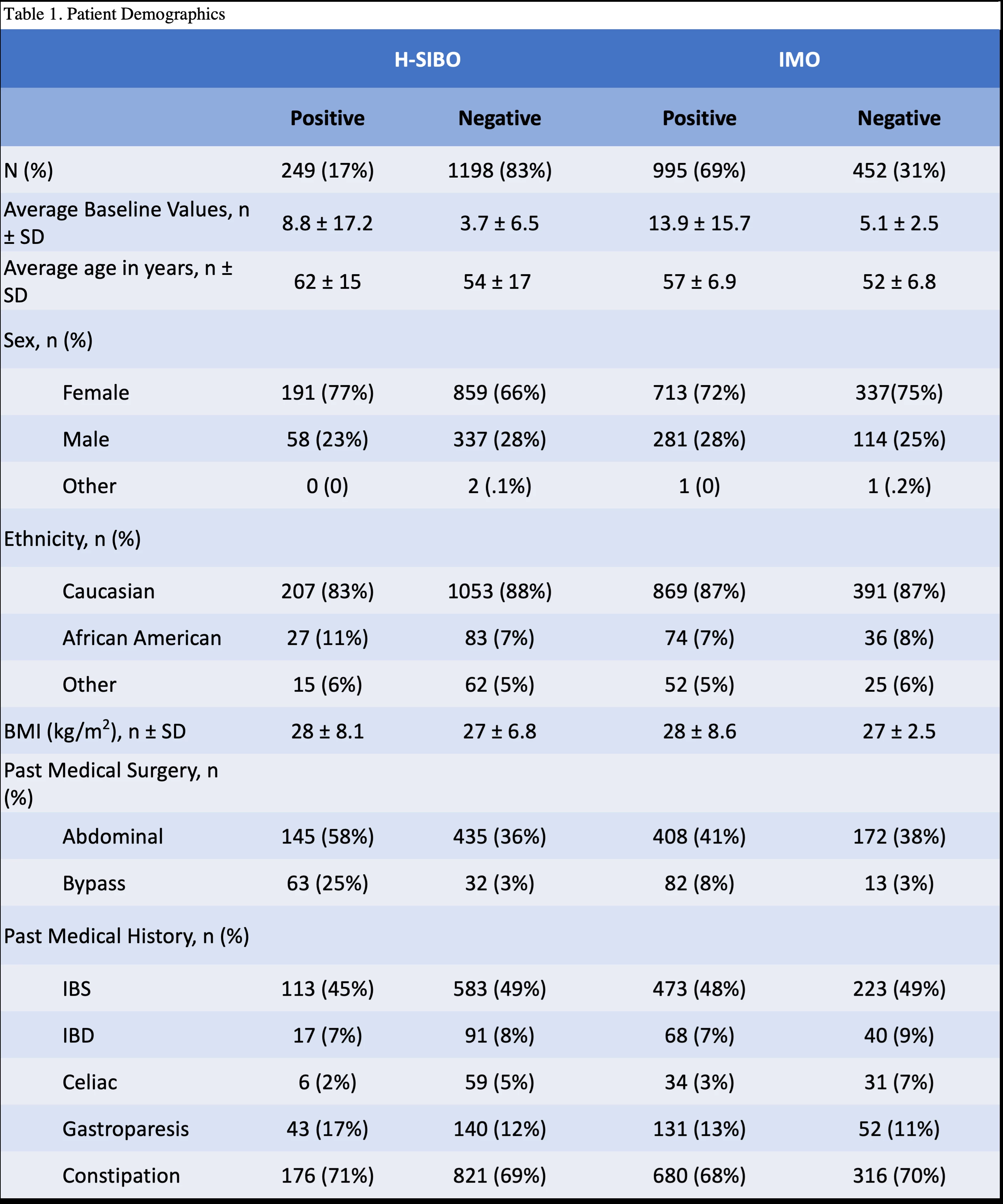
Table 1. Patient demographics

Table 2. Demographic and methane levels of IMO patients
Presenter
Other
AGA


